Physiology and pathology of shear stress in blood vessels
Responsible person: Jan Víteček
Vasculature is of extreme importance for maintenance of homeostasis throughout the whole body. Indeed, cardiovascular diseases are charged with the highest mortality burden in developed countries. Our focus is the connection between vascular inflammation and hemodynamics, thrombolysis in relation to ischemic stroke. Further we are interested in role of electrical gradients and currents in vascular homeostasis.
To understand many aspects of these phenomena, we are capitalizing on in vitro vasculature models. Fluidic models which range from simple chips with straight channels, to realistic, 3D patient data-based models are being optimized and utilized. To better understand aspects of ischemic stroke, static as well as fluidic models of thrombolysis have been introduced.
Vascular inflammation and hemodynamics
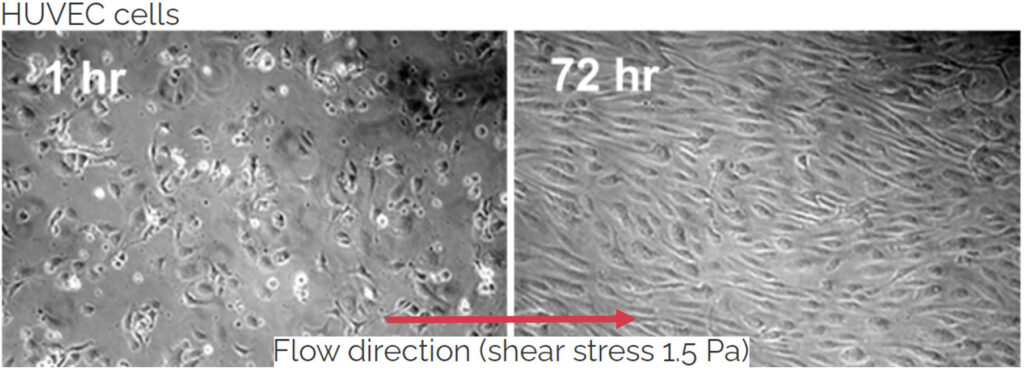
The vascular endothelium is a layer of specialized cell showing high degree of organization. The individual endothelial cell (EC) shows elongated shape mediated by highly organized actin filaments in the cytosol. Further ECs are oriented along with the blood flow. Tight junctions among cells mediate the primary function of vascular endothelium – regulation of vessel wall permeability which is under tight control and specific for a particular organ. Further the endothelial cells control vascular tone by means of sensing of shear stress (a coplanar force with the lumen of vessel wall which results from blood flow) and stimulating relaxation of smooth muscle cells in vessel wall by means of nitric oxide (NO) production. Importantly the endothelial cell layer regulates the immune response. Thus it is not surprising that the vascular endothelium is indispensable for homeostasis maintenance. Its dysfunction is a prerequisite for most of cardiovascular diseases including stroke and myocardial infarction. We are focused on studying the inflammation in microfluidic scale. On the other hand we employ 3D realistic models to study pathologies like intracranial aneurysms.
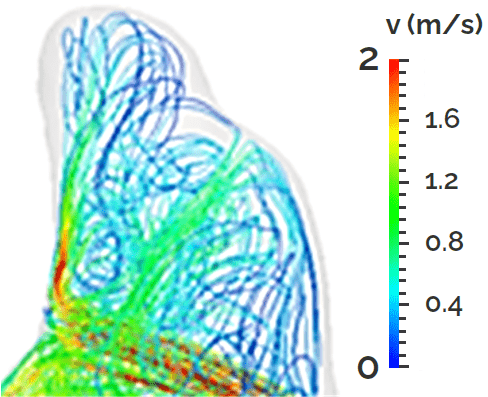

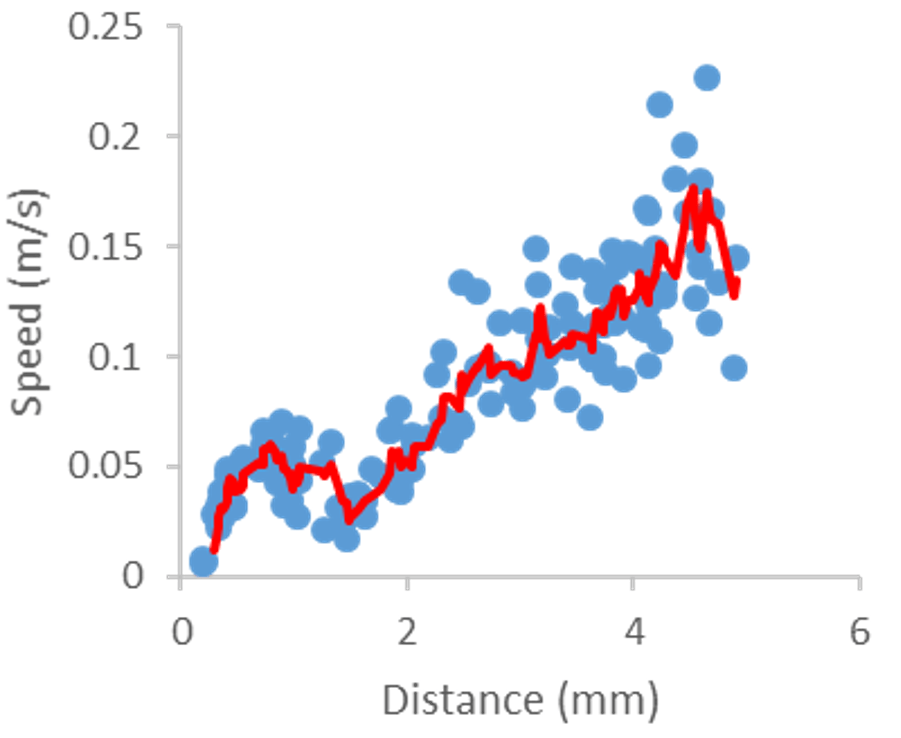
Comutational model of blood flow within an intracranial aneurysm (cooperation with Faculty of Mathematics and Physics, Charles University in Prague) and visualisation of the flow in laboratory model of such aneurysm together with evaluation of flow profile.